Glaucoma
Introduction to Glaucoma
Glaucoma results from nerve damage to the optic nerve by high eye pressure. The optic nerve connects the brain to the eye, and it is very sensitive to changes in eye pressure, also known as intraocular pressure (IOP). Most people consider ideal blood pressure to be around 120/80 mmHg, but eye pressure is highly individualized, and different people may develop glaucoma at different IOPs. At first, glaucoma damages peripheral (or side) vision, but most people would not detect this early peripheral visual loss. At more severe stages, peripheral vision loss spreads toward the center of vision, causing the so-called “tunnel vision.” At this severe stage, some patients may still be able to see 20/20 centrally and not realize the severity of their peripheral vision loss. Eventually, even the little bit of central vision can be lost if glaucoma is not treated. For these reasons, glaucoma is sometimes called “The Silent Thief of Sight.”
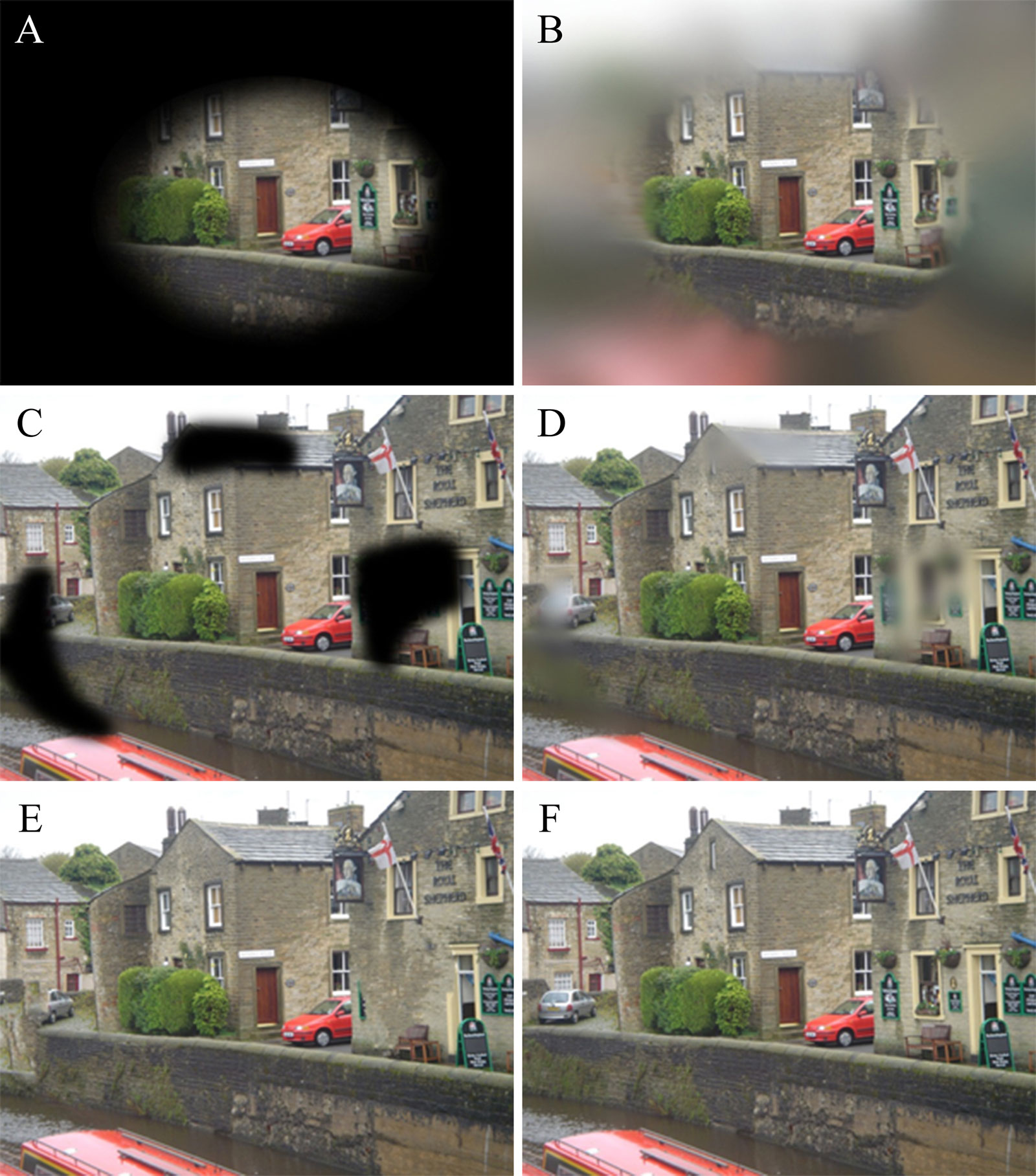
Images shown to the glaucoma patients during the study. These images were based upon commonly used simulations of glaucomatous visual field defects: black tunnel (A), blurred tunnel (B), black patches (C), blurred patches (D), missing parts (E), and no difference (F).
Source: “How Does Glaucoma Look? Patient Perception of Visual Field Loss” Ophthalmology, Vol. 120, Issue 6, pp. 1120-1126, June 2013
Glaucoma Testing
Vision Testing in the Clinic
Pachymetry
This test measures the thickness of the cornea, the transparent, front-most part of the eye. IOP is directly related to the thickness of the cornea. Thicker corneas tend to have falsely high IOPs, and thinner corneas tend to have falsely low IOPs. Each person’s IOP must be correlated with her corneal thickness.
Visual Field Test
As discussed above, peripheral vision is damaged first by glaucoma. The visual field test maps out the eye’s central and peripheral vision, and is used to track one’s visual field over time. It is done with one eye shut at a time, with the eye fixated at a central target, and takes about 4-7 minutes per eye depending on a person’s response time.
Gonioscopy
This is a test using a special contact lens on a person’s eye that has been anesthetized with eyedrops. Gonioscopy allows for viewing of the internal angle between the cornea and the iris (the colored part of the eye). This angle inside the eye is important in distinguishing between the different types of glaucoma, since medical treatment may vary depending on the type of glaucoma.
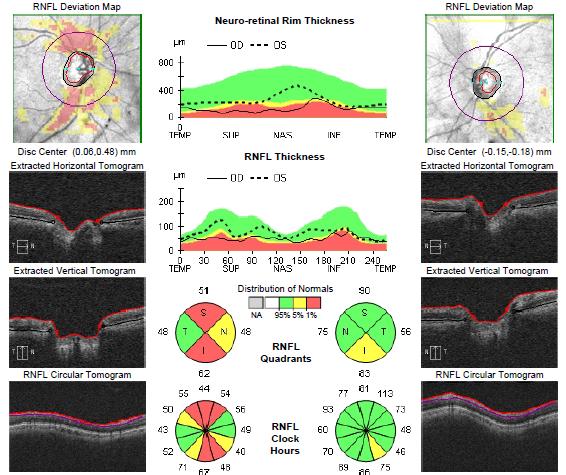
Optical Coherence Tomography (OCT)
The OCT uses light to digitally scan the optic nerve and measures its tissue thickness. This test is analogous to an ultrasound test, except that instead of using sound waves, it uses light rays to visualize the optic nerve. In glaucoma, the tissues of the optic nerve are compressed by high IOP and gradually become thinner. The OCT can be used to digitally track the optic nerve thickness and health over time.
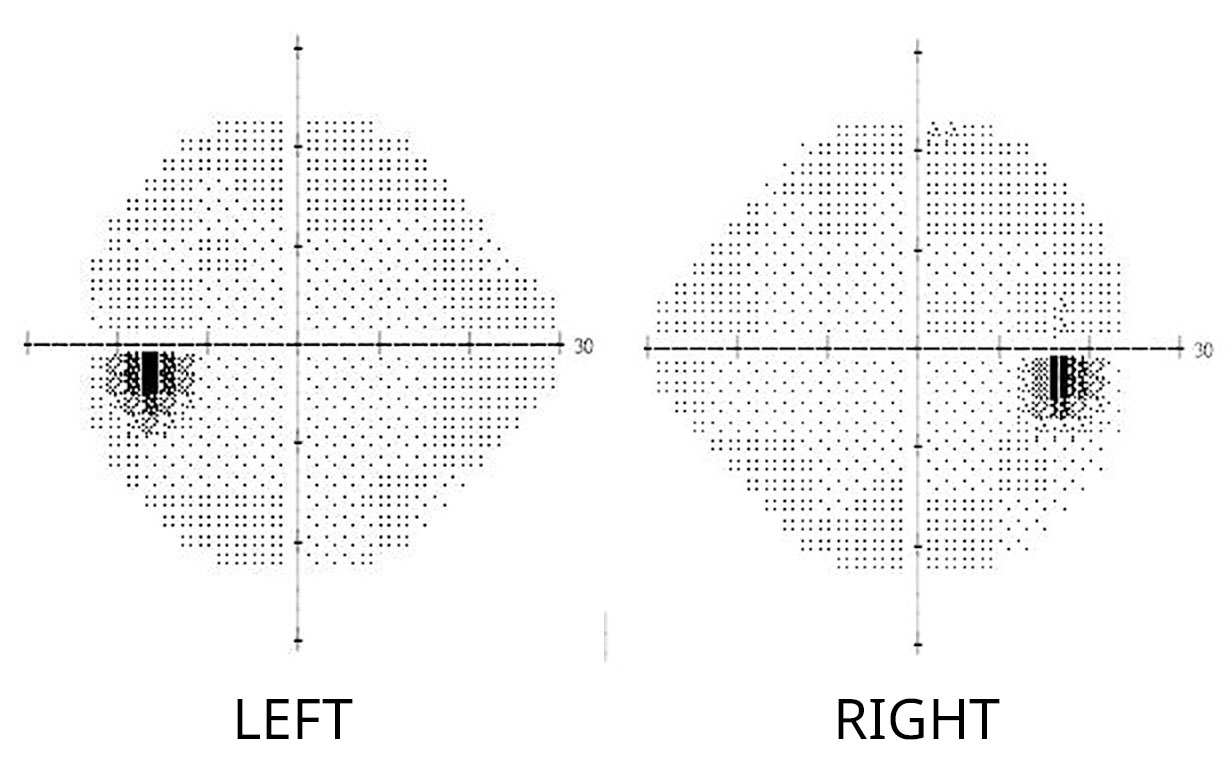
Example of a normal visual field. Note the natural “blind spots” in both eyes, where the blind spot is on the right side of the right eye, and on the left side of the left eye.
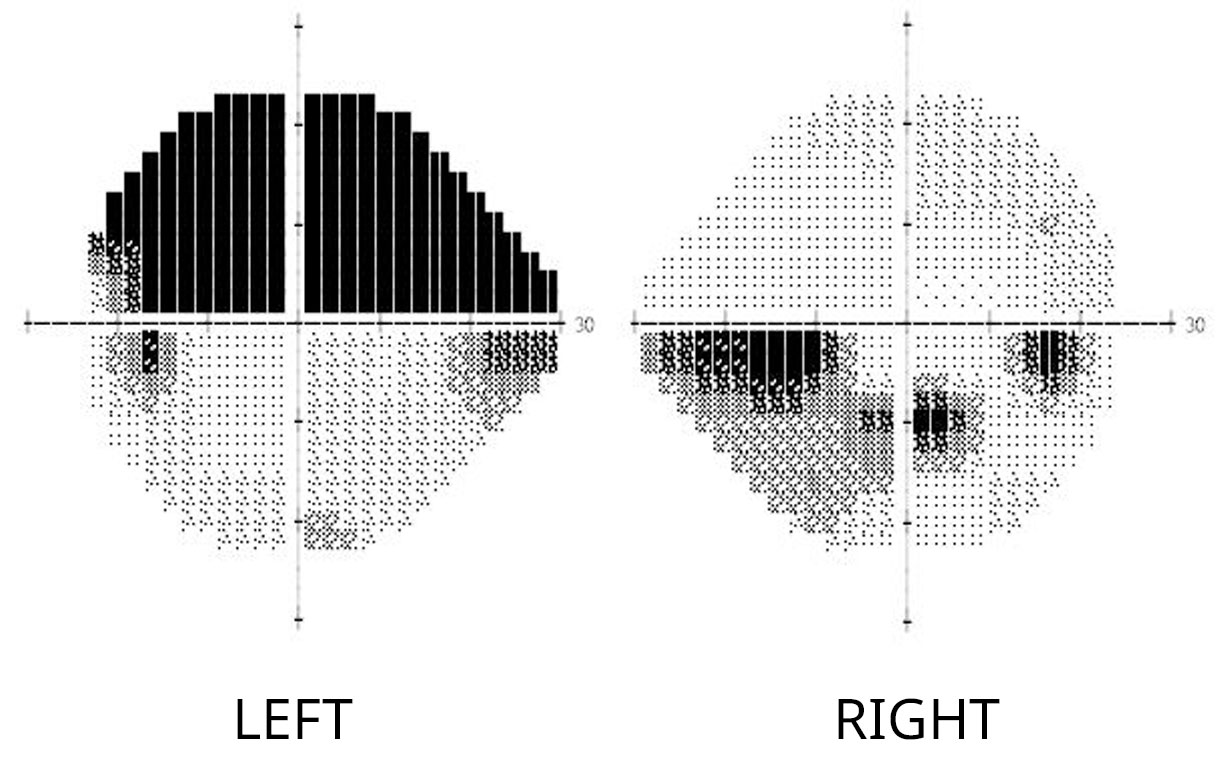
Example of moderate glaucomatous visual field loss. Note that besides the “blind spots,” dark areas representing loss of peripheral vision are evident in the upper half of the left eye and the lower left region of the right eye.
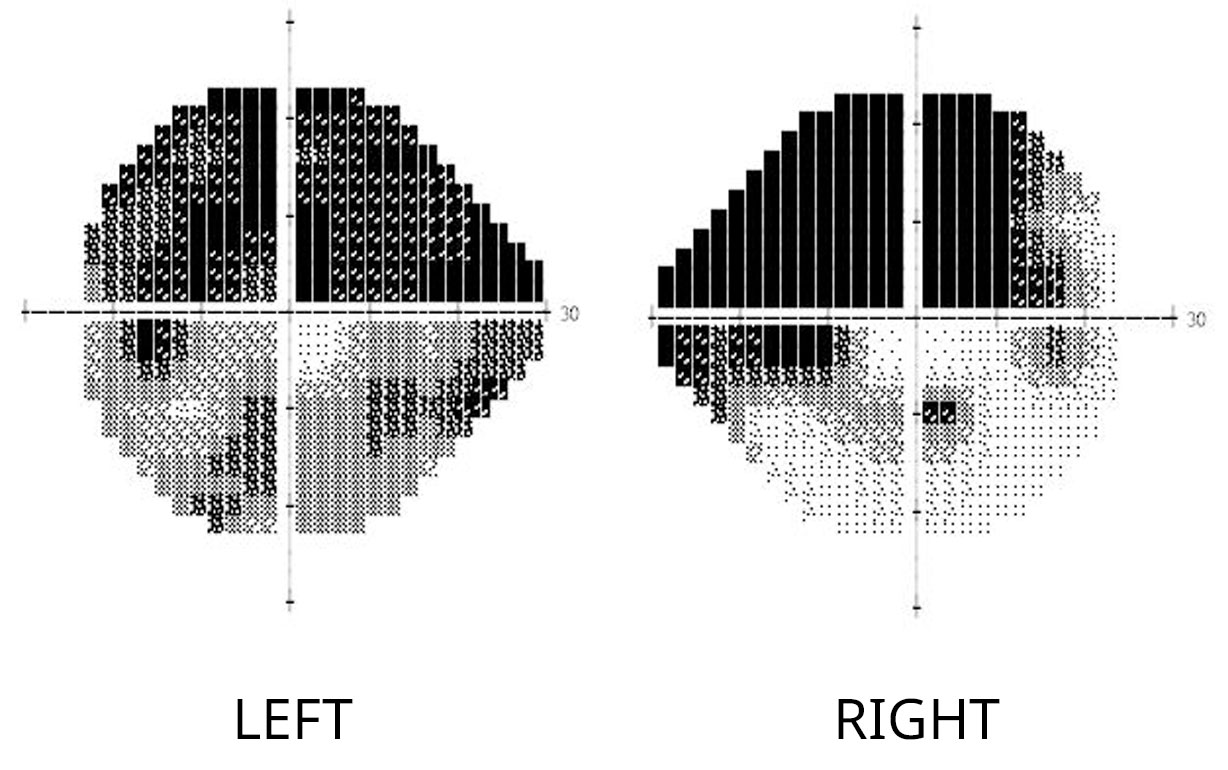
Example of severe glaucomatous visual field loss. Note the extensive peripheral field loss in the left eye, just sparing the central part of vision (represented by the central white area). This is the so called “tunnel vision” effect of glaucoma. On the right eye, note the extensive field loss in the upper half region as well as part of the lower half visual field.
Example of severe glaucomatous visual field loss. Note the extensive peripheral field loss in the left eye, just sparing the central part of vision (represented by the central white area). This is the so called “tunnel vision” effect of glaucoma. On the right eye, note the extensive field loss in the upper half region as well as part of the lower half visual field.
Glaucoma Treatment
Since the primary cause of glaucoma is high IOP, the treatment is to lower IOP to minimize optic nerve damage by the following methods:
1. Eyedrops:
Eyedrops are the first line treatment to lower IOP. Many medications are commercially available by prescription, and each has their unique side effect profile. Talk to your physician about the best medication for your glaucoma treatment.
2. Laser:
If eyedrops fail to adequately lower IOP, a laser procedure called trabeculoplasty can be performed to enhance the eye’s drainage system, thereby lowering the IOP. This procedure can be done in the office without going to the operating room, and only requires topical eyedrops to anesthetize the eye before starting the procedure.
3. Surgery:
If both eyedrops and laser trabeculoplasty fail to adequately lower one’s IOP, then surgical intervention is recommended to create a permanent diversion of fluid from inside the eye to its surrounding tissues to lower IOP. This procedure must be performed in the operating room.